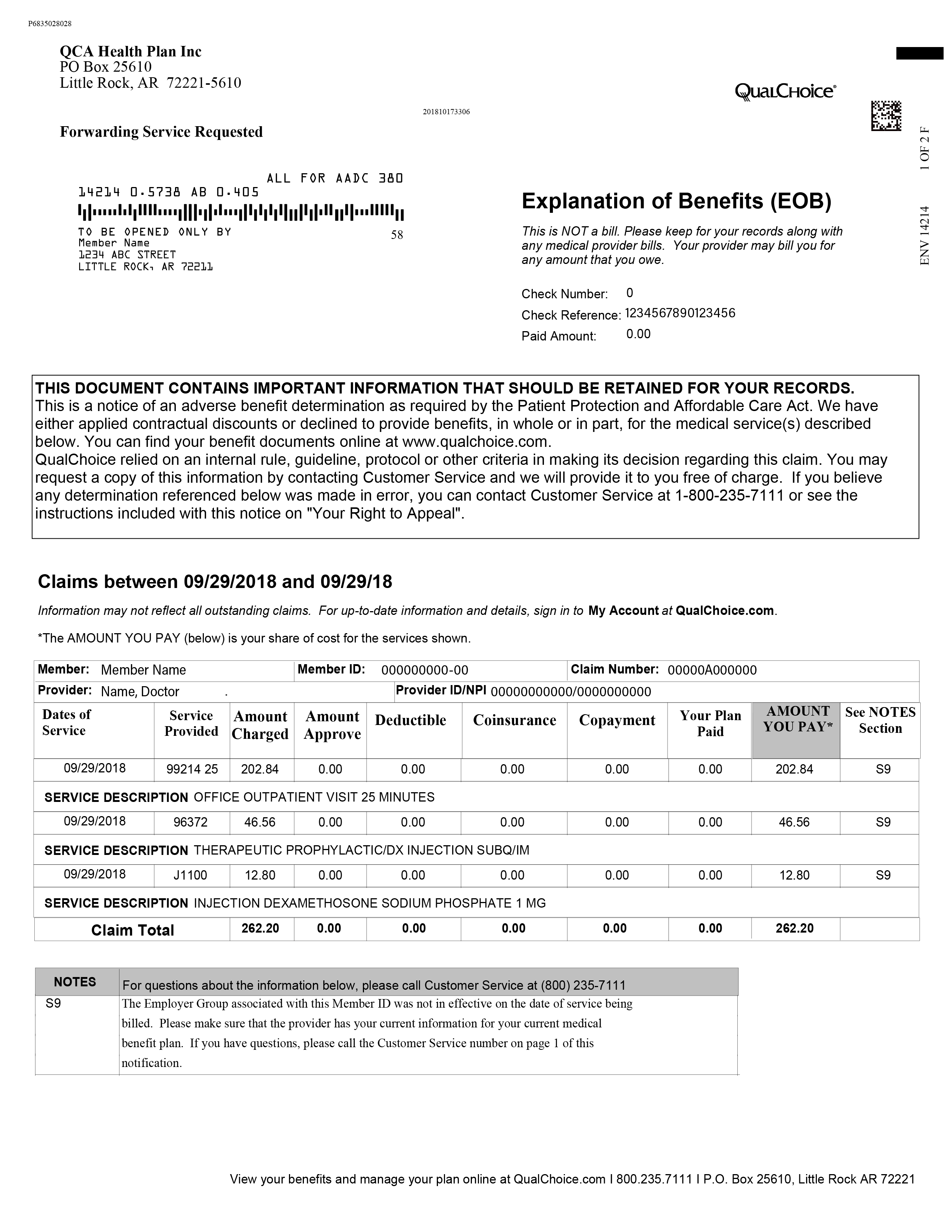
As a QualChoice member, you will receive an EOB every 14 days if you have had any claims during that time. Review the EOB closely and compare it to the receipt or statement from your doctor.* Keep it for your records, along with your medical bills.
The EOB is not a bill. It explains how your benefits were applied to your recent claims. Here’s what it shows:
- Date and type of service
- Amount charged
- Approved coverage amount
- Amount we paid
- Amount you must pay the provider
It also tells you how much has been applied toward your deductible, copayment or coinsurance.
How to Read the EOB Claim Details
We've numbered each item in the claim detail section of the EOB, below. Each item number is explained below.
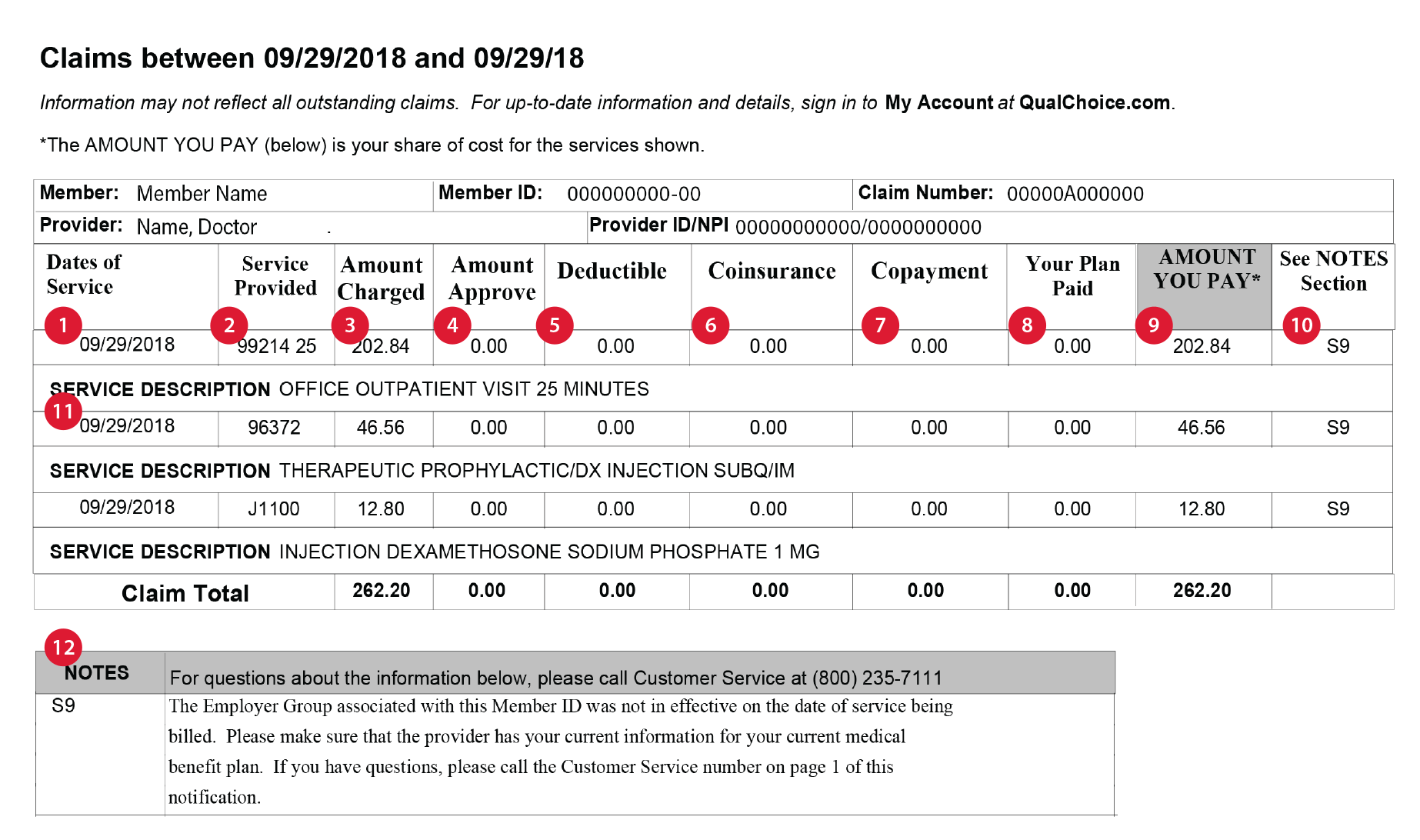
- Dates of Service: Date you received the medical care
- Service Provided: The medical code for the type of care you received
- Amount Charged: The amount the healthcare provider charged for the care
- Amount Approved: The amount QualChoice pays a provider for this type of care
- Deductible: The amount you pay for healthcare covered by your plan before QualChoice starts to pay
- Coinsurance: A fixed portion of the Maximum Allowable Charge you must pay toward the cost of certain covered services. Coinsurance has a maximum limit each year.
- Copayment: A fixed amount you pay for a covered service, usually at the time of service.
- Your Plan Paid: The amount QualChoice paid the provider
- Amount You Pay: The remaining amount that you must pay to the provider
- See NOTES Section: The claims code, which is explained in 12
- Service Description: A short explanation of exactly what the provider did
- NOTES: The reason why the claim was paid as it was, or not paid
To see what you’ve spent toward your deductible or out-of-pocket maximum and for the most up-to-date information: Sign in to My Account at QualChoice.com.
* Be sure to pay the provider the amount you see on your EOB, not the amount on their statement. If you continue to receive provider statements that disagree with your EOB, please contact the provider, then QualChoice Customer Service if needed.